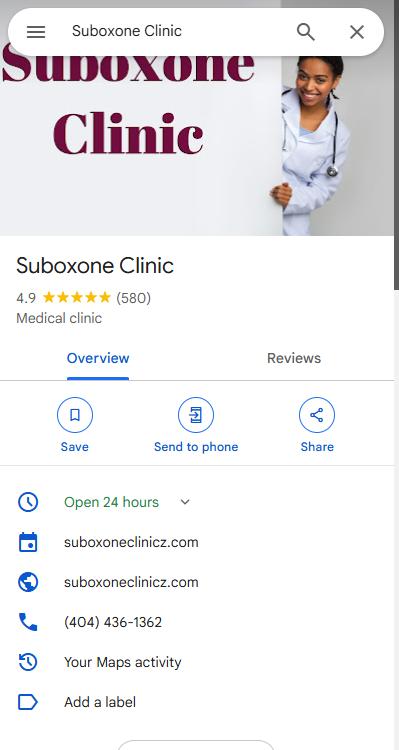
Suboxone Clinic
#1 Online Suboxone® clinic and Buprenorphine clinic in the United States.
Same day emergency telehealth treatments.
Schedule here
See a Suboxone® doctor from the comfort of your home Your Suboxone® (Generic Buprenorphine/Naloxone) will be sent electronically to a local pharmacy near you if you live in one of these states. If you live in other states your medication will be sent to our mail order pharmacy. They will deliver to your home within 2 days.
100% virtual and we see Patients from all over United States
Online suboxone Clinic


HOW IT WORKS


Step 1:
Register & Pay for your Suboxone clinic appointment
Step 2:
Video-Chat with our Medical Doctor
Step 3 :
Pick up your Suboxone at your local pharmacy 20 minutes later


Suboxone Doctor
Clinic communication is via Video-chat and text available 24/7 No commute, No traffic and No waiting.Same day appointments
Addiction counseling
Addiction therapy helps people to communicate their feelings without fear of being criticized or attacked.


Suboxone Clinic: A Beacon of Hope in the Fight Against Opioid Addiction
Opioid addiction is a growing public health crisis that has devastated communities and claimed countless lives. The need for effective treatment options has never been more urgent, and Suboxone clinics have emerged as a vital resource in the battle against opioid addiction. In this article, we will explore the role of Suboxone clinics in providing comprehensive care and support to individuals on their path to recovery.
Understanding Opioid Addiction
Opioid addiction is a chronic medical condition characterized by the compulsive use of opioids despite adverse consequences. Opioids, which include prescription painkillers and illegal drugs like heroin, can hijack the brain's reward system, making it incredibly difficult for individuals to quit using them. This addiction can lead to a range of devastating consequences, including health problems, strained relationships, and legal issues.
The Role of Suboxone
Suboxone, a brand name for the medication buprenorphine/naloxone, has become a cornerstone in the treatment of opioid addiction. It works by binding to the same receptors in the brain as opioids but with less euphoric and respiratory depressant effects. This makes it a valuable tool in managing cravings and withdrawal symptoms, allowing individuals to regain stability in their lives.
The Benefits of Suboxone Clinics
Suboxone clinics specialize in providing medication-assisted treatment (MAT) to individuals struggling with opioid addiction. These clinics offer a range of benefits that make them a critical component of the addiction treatment landscape:
1. Medically Supervised Treatment:
Suboxone clinics are staffed by medical professionals who can assess a patient's individual needs and adjust their treatment plan accordingly. This ensures a safe and effective recovery process.
2. Reduction in Cravings and Withdrawal Symptoms:
Suboxone helps manage cravings and alleviates the discomfort of opioid withdrawal, making it easier for individuals to focus on their recovery journey.
3. Reduced Risk of Overdose:
By stabilizing patients on Suboxone, the risk of fatal overdose is significantly reduced because the medication blocks the effects of other opioids.
4. Holistic Care:
Many Suboxone clinics offer a holistic approach to treatment, addressing not only the physical aspects of addiction but also the psychological and social factors that contribute to it. This may include counseling, therapy, and support groups.
5. Accessibility:
Suboxone clinics have become more widespread, increasing access to treatment for individuals in need. This accessibility is crucial in the fight against opioid addiction.
6. Long-term Maintenance:
Suboxone can be used as a long-term maintenance medication, allowing individuals to maintain their sobriety and reduce the risk of relapse.
The Stigma Surrounding MAT
Despite the proven effectiveness of Suboxone and other MAT options, there remains a stigma surrounding their use. Some people view MAT as merely replacing one addiction with another, but this oversimplification fails to acknowledge the complexities of addiction. Addiction is a medical condition that requires comprehensive treatment, and MAT is a valuable tool in that toolkit.
Conclusion
Suboxone clinics play a vital role in addressing the opioid addiction epidemic. They offer a safe and effective way for individuals to regain control of their lives and embark on a path to recovery. By providing medically supervised treatment, managing cravings and withdrawal symptoms, and addressing the holistic needs of patients, Suboxone clinics offer hope to those affected by opioid addiction. It's crucial that we continue to expand access to these clinics and challenge the stigma associated with medication-assisted treatment to save lives and combat this devastating public health crisis.
What is a Suboxone Clinic?
A Suboxone Clinic is a medical facility that specializes in the treatment of opioid addiction using Suboxone medication. Suboxone is a combination of buprenorphine and naloxone, which work together to reduce withdrawal symptoms and cravings for opioids. This Suboxone clinic provides patients with a comprehensive treatment program that includes medication-assisted treatment, counseling, and support services. The goal of the Suboxone Clinic is to help patients overcome opioid addiction and achieve long-term recovery. Treatment plans are customized for each patient based on their individual needs and medical history. The clinic's team of medical professionals, therapists, and support staff work together to provide patients with the highest level of care and support throughout their recovery journey.
How Do Suboxone Clinics Work?
Suboxone clinics work by utilizing medication-assisted treatment (MAT) with the prescription drug Suboxone, which contains buprenorphine and naloxone. Buprenorphine is a partial opioid agonist that helps reduce cravings and withdrawal symptoms, while naloxone is an opioid antagonist that discourages misuse. Patients typically receive Suboxone in a controlled setting and are monitored closely by medical professionals. The treatment also includes counseling and therapy to address the underlying issues contributing to substance use disorder. Suboxone clinics aim to provide a safe and effective way for individuals with opioid addiction to manage their cravings and withdrawal symptoms while addressing the root causes of their addiction. It is important to note that Suboxone clinics are not a cure for addiction, but rather an important tool in the recovery process.
Suboxone questions
How many Suboxone strips a day?
In Suboxone clinic the dosage and frequency of Suboxone strips should be determined by a qualified suboxone provider based on an individual's specific needs and circumstances. Suboxone is a medication used in the treatment of opioid dependence, and it contains a combination of buprenorphine and naloxone.
Typically, Suboxone treatment starts with an induction phase, during which the initial dose is carefully adjusted to alleviate withdrawal symptoms and reduce cravings without causing excessive sedation or intoxication. This phase is usually conducted under medical supervision.
Once the induction phase is complete, the maintenance phase begins. In this phase, the dose is typically stabilized and may be adjusted as needed. It is common for individuals to take a daily dose of Suboxone, often administered as a sublingual film or tablet.
What is the instruction on taking Suboxone?
Suboxone is a prescription medication primarily used for the treatment of opioid dependence. It contains two active ingredients: buprenorphine and naloxone. The following instructions provide a general guideline, but remember to follow the specific instructions provided by your doctor or pharmacist:
Prescription and dosage:
Suboxone is available in different strengths. Your healthcare provider will prescribe the appropriate dosage based on your individual needs. Always follow the prescribed dosage and do not modify it without consulting your doctor.
Administration:
Suboxone is usually taken sublingually, which means it is placed under the tongue and allowed to dissolve. It should not be chewed, swallowed, or crushed.
Preparation:
Ensure that your hands are dry before handling the Suboxone tablet or film. Take out the prescribed dose from its packaging.
Placement:
Place the tablet or film under your tongue or against the inside of your cheek. Let it dissolve completely without swallowing for the recommended duration.
Avoid food or drink:
Do not eat or drink while the Suboxone is dissolving, as it may affect the absorption of the medication.
Follow-up:
After the tablet or film has dissolved, you can swallow the remaining saliva. Do not rinse your mouth immediately after taking Suboxone, as it may interfere with absorption.
Frequency:
Suboxone is typically taken once daily. Follow your doctor's instructions regarding the exact timing and frequency of your doses.
Other medications:
Inform your healthcare provider about any other medications, supplements, or substances you are taking, as they may interact with Suboxone.
Does Suboxone prevent relapse?
Suboxone is a medication commonly used in the treatment of opioid dependence. It contains a combination of buprenorphine, a partial opioid agonist, and naloxone, an opioid antagonist. Suboxone helps manage withdrawal symptoms and cravings, making it easier for individuals to abstain from opioid use. While Suboxone can be an effective tool in opioid addiction treatment, it does not guarantee prevention of relapse on its own.
Relapse prevention involves multiple factors, including individual motivation, counseling, support networks, and lifestyle changes. Suboxone can assist in the early stages of recovery by reducing cravings and withdrawal symptoms, allowing individuals to focus on their recovery efforts. However, it is crucial to note that recovery from addiction is a complex and ongoing process that requires a comprehensive approach.
Suboxone is typically prescribed as part of a comprehensive treatment program that includes counseling and behavioral therapies. These therapies help individuals address the underlying issues contributing to their addiction, develop coping skills, and make positive changes in their lives. By combining medication-assisted treatment like Suboxone with counseling and support, individuals have a better chance of maintaining long-term recovery and reducing the risk of relapse.
How do you prevent precipitated withdrawal?
Precipitated withdrawal occurs when a person who is physically dependent on opioids suddenly goes into withdrawal after taking a medication called naloxone or another opioid antagonist. This can happen if the individual has opioids still bound to the opioid receptors in their body, and the antagonist displaces them abruptly, leading to rapid withdrawal symptoms.
To prevent precipitated withdrawal, it's crucial to follow proper protocols when administering medications that can precipitate withdrawal. Here are some guidelines to minimize the risk:
Ensure proper timing:
Wait until the opioids have sufficiently cleared from the person's system before administering an opioid antagonist. The precise timing depends on the half-life of the opioid they have taken. Generally, it is recommended to wait until the person exhibits clear signs of withdrawal, indicating that most of the opioids have been metabolized.
Use a withdrawal scoring system:
Assess the severity of withdrawal symptoms using a standardized scoring system, such as the Clinical Opiate Withdrawal Scale (COWS) or the Subjective Opiate Withdrawal Scale (SOWS). These scales help gauge the level of withdrawal and inform decisions on whether it is safe to administer an antagonist.
Start with a low dose:
When using an opioid antagonist, begin with a low dose to minimize the risk of precipitated withdrawal. By starting with a smaller amount, it allows for careful observation of the person's response. If there are no adverse reactions or signs of precipitated withdrawal, the dosage can be gradually increased if necessary.
Individualize the approach:
Each person's situation may vary, so it is essential to tailor the approach based on their specific needs and medical history. Consider factors such as the type and dose of opioids previously used, the duration of use, and the person's overall health.
Consult healthcare professionals:
If you are uncertain or unfamiliar with the process of preventing precipitated withdrawal, it is strongly advised to seek guidance from healthcare professionals who specialize in addiction medicine or pain management. They can provide personalized advice based on the individual's circumstances.
What are the side effects of Suboxone?
Suboxone is a prescription medication used in the treatment of opioid dependence. It contains a combination of buprenorphine and naloxone. Like any medication, Suboxone can have potential side effects. Common side effects include:
Nausea and vomiting
Headache
Constipation
Insomnia or disturbed sleep
Sweating
Dizziness or lightheadedness
Stomach pain
Back pain
Fatigue or weakness
Irregular heartbeat or palpitations
Less common, but more serious side effects can occur, and if you experience any of these, it is important to seek medical attention:
Allergic reactions, such as hives, rash, itching, swelling, severe dizziness, or difficulty breathing.
Respiratory problems, including slowed or shallow breathing.
Liver problems, which may manifest as yellowing of the skin or eyes (jaundice), dark urine, or persistent nausea or vomiting.
Adrenal insufficiency, which can lead to symptoms like fatigue, weakness, loss of appetite, dizziness, or low blood pressure.
Does buprenorphine alone cause precipitated withdrawals?
No, buprenorphine alone does not typically cause precipitated withdrawals. Precipitated withdrawals occur when a person who is physically dependent on full agonist opioids, such as heroin or oxycodone, takes buprenorphine or another partial agonist opioid. This is because buprenorphine has a higher affinity for opioid receptors and can displace the other opioids, leading to a sudden onset of withdrawal symptoms.
Is Suboxone a good pain reliever?
Suboxone (buprenorphine/naloxone) is primarily used for the treatment of opioid dependence and addiction. It is not typically prescribed as a first-line medication for pain relief. However, buprenorphine, one of the active ingredients in Suboxone, does possess analgesic properties and can provide some pain relief.
Buprenorphine is a partial opioid agonist, meaning it binds to opioid receptors in the brain but produces a weaker effect compared to full opioid agonists like morphine or oxycodone. It can be effective in managing moderate to severe pain in certain situations, such as in cases where a person has a history of opioid dependence or addiction.
It's important to note that Suboxone is a combination medication containing buprenorphine and naloxone. Naloxone is added to deter misuse of the medication by individuals attempting to inject or misuse it. The presence of naloxone does not significantly affect the analgesic properties of buprenorphine.
Is it better to take Suboxone once a day?
The dosing regimen for Suboxone, a medication used for opioid dependence, is typically determined by a Suboxone doctor based on individual needs and circumstances. However, it is commonly prescribed to be taken once a day.
Suboxone contains buprenorphine and naloxone. Buprenorphine is a partial opioid agonist that helps alleviate withdrawal symptoms and cravings associated with opioid addiction. Naloxone is included to deter misuse by individuals who may attempt to inject or misuse the medication.
The once-daily dosing of Suboxone offers several advantages. It helps maintain steady levels of buprenorphine in the body, reducing fluctuations in drug levels and minimizing withdrawal symptoms. It also simplifies the medication regimen, making it more convenient for patients.
Is Suboxone a good pain reliever?
Suboxone (buprenorphine/naloxone) is primarily used for the treatment of opioid dependence and addiction. It is not typically prescribed as a first-line medication for pain relief. However, buprenorphine, one of the active ingredients in Suboxone, does possess analgesic properties and can provide some pain relief.
Buprenorphine is a partial opioid agonist, meaning it binds to opioid receptors in the brain but produces a weaker effect compared to full opioid agonists like morphine or oxycodone. It can be effective in managing moderate to severe pain in certain situations, such as in cases where a person has a history of opioid dependence or addiction.
It's important to note that Suboxone is a combination medication containing buprenorphine and naloxone. Naloxone is added to deter misuse of the medication by individuals attempting to inject or misuse it. The presence of naloxone does not significantly affect the analgesic properties of buprenorphine.
When should I start taking SUBOXONE?
The decision to start taking Suboxone should be made in consultation with a healthcare professional, typically a doctor who specializes in addiction medicine. They will evaluate your specific situation, including the severity of your opioid dependence and any other factors that may be relevant to determine if Suboxone is an appropriate treatment option for you.
In general, Suboxone is often used as part of a comprehensive treatment program that may include counseling, behavioral therapy, and support groups. It is typically prescribed to individuals who are already experiencing withdrawal symptoms or are in the early stages of opioid detoxification.
What is the action of SUBOXONE?
Suboxone is a medication used in the treatment of opioid dependence and addiction. It is a combination medication containing two active ingredients: buprenorphine and naloxone.
Buprenorphine is a partial opioid agonist, which means it binds to the opioid receptors in the brain but produces a milder effect compared to full opioid agonists like heroin or oxycodone. By occupying the opioid receptors, buprenorphine helps to alleviate withdrawal symptoms and reduce cravings for opioids. It can also help to normalize brain function, allowing individuals to engage in daily activities without the disruptive effects of opioid use.
Naloxone, the second active ingredient in Suboxone, is an opioid antagonist. It blocks the effects of opioids by binding to the same receptors but without activating them. Naloxone is primarily included in Suboxone to deter misuse. When taken as directed (sublingually, by dissolving the tablet under the tongue), the naloxone has minimal effect. However, if Suboxone is crushed and injected, the naloxone component becomes active and can precipitate withdrawal symptoms in individuals who are dependent on opioids. This serves as a deterrent against intravenous use of Suboxone.
The combination of buprenorphine and naloxone in Suboxone helps to manage opioid dependence by reducing withdrawal symptoms, suppressing cravings, and discouraging misuse of the medication. It is typically used as part of a comprehensive treatment plan that includes counseling and behavioral therapy to support individuals in their recovery from opioid addiction.
What kind of drug is SUBOXONE?
Suboxone is a medication used in the treatment of opioid dependence and addiction. It is a combination medication that contains two active ingredients: buprenorphine and naloxone.
Buprenorphine is a partial opioid agonist, which means it activates opioid receptors in the brain but produces a weaker effect compared to full opioid agonists like heroin or oxycodone. It helps to relieve withdrawal symptoms and reduce cravings for opioids without producing the intense euphoria associated with other opioids.
Naloxone, on the other hand, is an opioid antagonist. It blocks the effects of opioids and can precipitate withdrawal symptoms if taken by individuals dependent on opioids. Naloxone is included in Suboxone as a safety measure to deter misuse of the medication.
Suboxone is typically administered as a sublingual film or tablet that dissolves under the tongue. It is usually prescribed as part of a comprehensive treatment program that includes counseling and psychosocial support to help individuals recover from opioid addiction.
Is Suboxone good for pain?
Suboxone is primarily used for treating opioid dependence and addiction. It contains two active ingredients, buprenorphine and naloxone, which work together to reduce cravings and withdrawal symptoms in individuals who are dependent on opioids.
While buprenorphine, one of the components of Suboxone, is an opioid itself, it has a partial agonist effect on the opioid receptors in the brain, which means it produces milder opioid effects compared to full agonists like heroin or oxycodone. Due to its unique properties, Suboxone is not typically prescribed for pain management.
If you are experiencing pain and seeking appropriate treatment, it is important to consult with a healthcare professional who can evaluate your specific situation and recommend suitable options for pain relief. There are various alternative medications and therapies available that can address different types of pain effectively.
How do you take SUBOXONE film?
SUBOXONE film is a prescription medication used to treat opioid dependence. It contains two active ingredients: buprenorphine and naloxone. It comes in the form of a dissolvable film that is placed under the tongue or inside the cheek. Here's a general guide on how to take SUBOXONE film:
Wash your hands: Before handling the film, make sure to wash your hands thoroughly with soap and water to maintain good hygiene.
Open the package: Tear open the individual blister package containing the SUBOXONE film. Be careful not to push the film out or damage it while opening.
Prepare your mouth: Make sure your mouth is clean and dry. Avoid eating or drinking anything for at least 15 minutes before taking the medication.
Place the film under your tongue or inside your cheek: Gently place the SUBOXONE film under your tongue or inside your cheek. The medication will dissolve on its own. If placing under the tongue, try to position it so that it's touching the floor of your mouth, as this can help with absorption.
Allow the film to dissolve: Let the film dissolve completely without chewing or swallowing it. This process usually takes 2 to 10 minutes. Avoid talking or moving your tongue excessively during this time to allow for proper absorption.
Avoid eating or drinking: Try not to eat or drink anything until the film has completely dissolved. This usually takes around 30 minutes. Eating, drinking, or smoking during this time may reduce the effectiveness of the medication.
Dispose of the film: After the film has dissolved, you can swallow any remaining saliva. If there are any film remnants left, you can dispose of them in a responsible manner, such as by flushing them down the toilet as instructed by your healthcare provider or pharmacist.
The rising popularity of suboxone clinics in addiction treatment
Suboxone clinics had been gaining popularity in addiction treatment due to their effectiveness in managing opioid dependence and promoting recovery. Suboxone, a brand name for the medication containing buprenorphine and naloxone, is used as a medication-assisted treatment (MAT) for opioid use disorder (OUD).
The rising popularity of Suboxone clinics can be attributed to several factors:
Medication-assisted treatment (MAT) efficacy: Suboxone has shown promising results in reducing cravings, withdrawal symptoms, and illicit opioid use. It helps stabilize individuals, enabling them to participate more effectively in their treatment and other aspects of their lives.
Reduced stigma: The concept of MAT has become more widely accepted as a treatment approach for addiction, reducing the stigma associated with seeking help for opioid use disorder.
Accessibility: The establishment of specialized Suboxone clinics has increased access to this treatment for individuals struggling with opioid addiction. These clinics are often staffed with medical professionals trained in addiction medicine.
Holistic approach: Many Suboxone clinics adopt a comprehensive approach to addiction treatment, incorporating counseling, therapy, and support groups alongside medication management. This combination addresses both the physical and psychological aspects of addiction, enhancing the chances of long-term recovery.
Regulatory support: Governments and healthcare authorities in many countries have recognized the importance of expanding access to MAT for opioid addiction. They have taken steps to reduce barriers and facilitate the establishment of Suboxone clinics.
Lower risk of overdose and diversion: Suboxone has a lower risk of overdose compared to full opioid agonists like heroin or prescription opioids. The inclusion of naloxone in Suboxone helps deter misuse, as naloxone can precipitate withdrawal symptoms if the medication is misused.
It's important to note that the situation may have evolved since my last update, and the popularity and acceptance of Suboxone clinics may have continued to grow. However, it's also essential to acknowledge that addiction treatment is a complex and evolving field, and different approaches may be more suitable for different individuals.
Suboxone vs. methadone: a comparison of opioid addiction treatments
Suboxone and methadone are both medications used to treat opioid addiction, but they have some key differences in their composition, administration, and overall approach to treatment. Let's compare them based on various factors:
Composition:
Suboxone: It is a combination medication containing buprenorphine and naloxone. Buprenorphine is a partial opioid agonist, which means it activates opioid receptors in the brain but to a lesser extent than full opioid agonists like heroin or oxycodone. Naloxone is an opioid antagonist, which is added to deter abuse of the medication.
Methadone: It is a full opioid agonist, meaning it fully activates opioid receptors in the brain. It is a synthetic opioid, similar to morphine but with a longer duration of action.
Administration:
Suboxone: It is usually taken as a sublingual film or tablet, dissolved under the tongue.
Methadone: It is typically dispensed in liquid form and taken orally.
Regulation:
Suboxone: In some countries, Suboxone can be prescribed by qualified physicians who have undergone specific training for opioid addiction treatment.
Methadone: It is typically dispensed through specialized clinics that are specifically licensed to provide methadone treatment.
Dosage Frequency:
Suboxone: It is often taken once daily or every other day, depending on the patient's needs and the stage of treatment.
Methadone: Initially, it is taken daily, and as the patient stabilizes, some clinics may allow take-home doses several times a week.
Withdrawal Management:
Suboxone: It can help manage withdrawal symptoms and reduce cravings without providing the intense euphoria of full opioids.
Methadone: It also helps with withdrawal symptoms and reduces cravings by satisfying the body's need for opioids.
Risk of Overdose:
Suboxone: It has a lower risk of overdose compared to full opioids because of the ceiling effect of buprenorphine. Taking more Suboxone than prescribed does not produce stronger effects.
Methadone: There is a higher risk of overdose, particularly during the early stages of treatment when tolerance is not yet established.
Addiction Potential:
Suboxone: It still carries a risk of dependence, but the risk is generally lower compared to full opioids.
Methadone: It has a higher addiction potential due to its full opioid agonist properties.
Treatment Duration:
Suboxone: Treatment duration can vary based on individual needs and progress but can extend for months to years.
Methadone: Treatment duration may also vary but is often considered long-term or indefinite for some individuals.
Both Suboxone and methadone have their advantages and disadvantages, and the choice between the two depends on the individual's medical history, severity of addiction, and specific treatment goalseffectively.
What is the role of suboxone clinics in the opioid epidemic?
Suboxone clinics play a crucial role in addressing the opioid epidemic, which has been a significant public health crisis in many parts of the world. Suboxone, also known by its generic name buprenorphine/naloxone, is a medication commonly used in medication-assisted treatment (MAT) for opioid use disorder (OUD). Opioid use disorder involves a problematic pattern of opioid use that leads to impairment or distress.
The role of suboxone clinics in the opioid epidemic includes several key aspects:
Medication-Assisted Treatment (MAT): Suboxone is an FDA-approved medication for treating opioid use disorder. It works by activating the same receptors in the brain that opioids target, but it produces milder effects and reduces withdrawal symptoms and cravings. Suboxone clinics provide MAT services, which involve prescribing and monitoring the use of suboxone as part of a comprehensive treatment plan.
Reducing Withdrawal Symptoms: One of the main reasons individuals with opioid use disorder struggle to quit opioids is the intense withdrawal symptoms that occur when they stop using. Suboxone helps manage these withdrawal symptoms, making it easier for individuals to transition away from more harmful opioids.
Minimizing Cravings: Opioid cravings can be incredibly powerful and can lead to relapse even after an individual has detoxed. Suboxone helps reduce these cravings, allowing individuals to focus on their recovery without constantly battling the urge to use opioids.
Harm Reduction: Suboxone clinics contribute to harm reduction efforts by providing a safer alternative to illicit opioids. Since suboxone is administered under medical supervision, it reduces the risk of overdose and the transmission of infectious diseases associated with injecting opioids.
Medical Supervision and Support: Suboxone clinics offer a supportive and structured environment for individuals seeking treatment. Medical professionals at these clinics can monitor patients' progress, adjust medication dosages, and provide counseling and behavioral therapy to address the underlying factors contributing to opioid use disorder.
Integration of Services: Suboxone clinics often integrate medical, psychological, and social services to provide comprehensive care. This holistic approach addresses not only the physical aspects of addiction but also the psychological, emotional, and social factors that can contribute to continued opioid use.
Stigma Reduction: Suboxone clinics contribute to reducing the stigma associated with opioid addiction. By treating addiction as a medical condition and offering evidence-based treatments, these clinics help shift the narrative around addiction and encourage individuals to seek help without fear of judgment.
Long-Term Management: Opioid use disorder is a chronic condition that requires ongoing management. Suboxone clinics support patients in the long-term management of their addiction, helping them maintain their recovery and prevent relapse.
In summary, suboxone clinics are an essential component of the comprehensive response to the opioid epidemic. By providing evidence-based medication-assisted treatment, they help individuals with opioid use disorder manage withdrawal symptoms, cravings, and the various challenges associated with addiction, ultimately improving their chances of achieving sustained recovery.
The effectiveness of suboxone in opioid withdrawal management
Suboxone, a brand name for a medication containing buprenorphine and naloxone, is commonly used in opioid withdrawal management and opioid use disorder treatment. Buprenorphine is a partial opioid agonist, which means it activates opioid receptors in the brain to a lesser extent compared to full agonists like heroin or oxycodone. Naloxone is included in the medication to deter misuse by injection, as naloxone can precipitate withdrawal symptoms in individuals who are opioid-dependent.
The effectiveness of Suboxone in opioid withdrawal management can be significant for several reasons:
Reduced Withdrawal Symptoms: Suboxone helps alleviate withdrawal symptoms that can be extremely uncomfortable and distressing during opioid withdrawal. Its partial agonist activity can help ease cravings and the physical discomfort associated with withdrawal.
Smoother Transition: Since Suboxone is a partial agonist, it provides a controlled and gradual reduction of the opioid effect, which can result in a smoother transition during detoxification compared to going "cold turkey."
Reduced Cravings: The partial agonist action of buprenorphine can help reduce cravings for stronger opioids, making it easier for individuals to resist relapse and focus on recovery.
Less Intense Euphoria: Buprenorphine's partial agonist activity produces a ceiling effect on the opioid high, making it less likely for individuals to misuse it to achieve a euphoric state.
Longer Duration of Action: Suboxone has a longer duration of action compared to other opioids, allowing for once-daily dosing. This reduces the need for frequent dosing and minimizes the likelihood of missed doses and subsequent withdrawal.
Lower Risk of Overdose: Suboxone has a safety advantage over full opioid agonists. The presence of naloxone discourages injection misuse, and even if taken sublingually (under the tongue) as directed, the ceiling effect of buprenorphine makes it less likely to cause respiratory depression and overdose.
Psychosocial Support: Suboxone treatment is often accompanied by psychosocial support, counseling, and therapy, which can enhance its effectiveness by addressing the psychological aspects of opioid use disorder.
Accessibility: Suboxone can be prescribed by qualified healthcare providers, such as doctors who have obtained a special waiver to prescribe buprenorphine for opioid use disorder treatment. This increases its availability and accessibility for patients seeking treatment.
50 trending topics on opioid addiction
The Opioid Epidemic: Current State and Impact
Opioid Addiction Treatment Options
Opioid Overdose and Prevention Strategies
Prescription Opioid Misuse and Abuse
Heroin Use and its Connection to Opioid Epidemic
Fentanyl Crisis and its Lethal Impact
Opioid Addiction in Adolescents and Young Adults
Opioid Withdrawal Symptoms and Management
Long-term Effects of Opioid Abuse
Opioid Use Disorder and Co-Occurring Mental Health Issues
Opioid Addiction and Homelessness
Role of Naloxone in Overdose Reversal
Stigma and Opioid Addiction: Breaking Barriers to Treatment
Opioid Addiction in Rural Communities
Opioid Prescribing Guidelines and Practices
Opioid Addiction among Veterans
Role of Opioids in Chronic Pain Management
Opioid Addiction in the LGBTQ+ Community
Neonatal Abstinence Syndrome (NAS)
Opioid Addiction and Pregnancy
Opioid Addiction in the Workplace
Opioid Treatment Programs: Methadone vs. Buprenorphine
Opioid Addiction and Criminal Justice System
Opioid Crisis and Opioid Litigation
Opioid Addiction and Social Media Influence
Opioid Addiction in the Elderly Population
Opioid Addiction and Genetics
Opioid Addiction and the Role of Healthcare Providers
Opioid Addiction and Drug Interactions
Opioid Addiction and HIV/AIDS
Opioid Addiction and Hepatitis C
Opioid Addiction and Drug Trafficking
Opioid Addiction and the Impact on Families
Opioid Addiction and Mental Health Stigma
Opioid Addiction and the Role of Pharmacies
Opioid Addiction and Peer Support
Opioid Addiction and the Role of Education
Opioid Addiction and the Pharmaceutical Industry
Opioid Addiction and Alternative Pain Management Techniques
Opioid Addiction and Access to Treatment
Opioid Addiction and International Perspectives
Opioid Addiction and the Impact on Foster Care Systems
Opioid Addiction and Chronic Illness Management
Opioid Addiction and Drug Policy Reform
Opioid Addiction and Naloxone Distribution Programs
Opioid Addiction and Prescription Drug Monitoring Programs (PDMPs)
Opioid Addiction and Medication-Assisted Treatment (MAT)
Opioid Addiction and Opioid Replacement Therapies
Opioid Addiction and Opioid-related Suicides
Opioid Addiction and the Impact on the LGBTQ+ Community
50 trending topics on suboxone clinic
Advancements in Suboxone treatment protocols
The role of Suboxone clinics in addressing the opioid epidemic
Telemedicine and virtual consultations in Suboxone clinics
Government policies and funding for Suboxone clinics
The impact of Suboxone clinics on reducing opioid overdose rates
Integrative approaches to addiction treatment in Suboxone clinics
Access to Suboxone clinics in rural areas
Suboxone and pregnancy: Benefits and risks
Suboxone treatment for adolescents and young adults
Challenges in tapering off Suboxone
Combining therapy with Suboxone treatment
Addressing stigma around Suboxone clinics and medication-assisted treatment
The economics of Suboxone treatment
Suboxone clinics and harm reduction strategies
Insurance coverage and affordability for Suboxone treatment
Dual diagnosis: Treating co-occurring mental health disorders with Suboxone
Long-term effects of Suboxone use
Opioid detoxification vs. Suboxone maintenance treatment
Suboxone for chronic pain management
The role of family support in Suboxone treatment
Suboxone clinics and relapse prevention strategies
Opioid withdrawal management with Suboxone
Suboxone clinics and community outreach programs
Cultural competence in Suboxone treatment
Suboxone and its impact on liver health
Peer support in Suboxone clinics
Suboxone clinics and medication diversion prevention
Overcoming barriers to entering Suboxone treatment programs
The future of Suboxone treatment: Innovations and research
Suboxone clinics and harm reduction strategies
Addressing opioid use disorder in the elderly population with Suboxone
Suboxone treatment in correctional facilities
Suboxone and its impact on sleep patterns
Addiction recovery apps and tools for Suboxone patients
Mindfulness and Suboxone treatment
Suboxone clinics and outreach to homeless populations
Suboxone treatment during the COVID-19 pandemic
Naloxone and its role in conjunction with Suboxone treatment
Medication-assisted treatment and 12-step programs
Suboxone clinics and LGBTQ+ inclusive care
Suboxone and its effect on cognitive function
Patient satisfaction and outcomes in Suboxone clinics
Addressing treatment disparities in Suboxone clinics
Suboxone clinics and harm reduction in party scenes and music festivals
Suboxone treatment for incarcerated individuals upon release
Suboxone and its impact on fertility and reproductive health
Suboxone clinics and employer support programs
Managing chronic pain after completing Suboxone treatment
Suboxone and the risk of overdose during relapse
The integration of technology in Suboxone clinics: Telehealth, wearables, and data tracking
How big is a Suboxone strip?
Does Suboxone make you sleep a lot?
How do you get rid of a Suboxone headache?
Is Suboxone a controlled substance?
How long should I be on Suboxone?
Do I get suboxone on the first visit?
Can I be fired for being a recovering opioid addict?
Can a hospital prescribe Suboxone?
which one is better: Tablet or strip? Is Suboxone film stronger than the pill?
what are other treatment options
what is addiction?
Vicodin Addiction; What you need to know
How can I get emergency Suboxone?
,,,,
....
......
What’s the Difference between Subutex and Suboxone?
what are Benefits of Suboxone?
what are Suboxone Uses, Side Effects, & Addiction?
What Drugs Can Interact With Suboxone?
what's the effect of alcohol and suboxone
Can You Overdose on Suboxone?
Does Suboxone change your personality?
What else is Suboxone used for? Is Suboxone used for chronic pain?
Is Suboxone same as Buprenorphine?
Does buprenorphine cause mania?
Why place Subutex/suboxone under the tongue?
Does buprenorphine cause memory loss?
Does Subutex still work if you swallow it?
Can you skip a day of Suboxone?
3750 N Henry Blvd Stockbridge GA 30281